Example of Nurses Notes: Real-Life Documentation Insights

Effective Nurse Notes Documentation: Real-Life Examples & Best Practices
Nurse notes are the backbone of patient care, providing critical insights into a patient’s condition, treatment, and progress. Accurate and detailed documentation ensures continuity of care, supports legal compliance, and enhances patient outcomes. Whether you’re a seasoned nurse or a student, understanding how to write effective nurse notes is essential. Below, we explore real-life examples and actionable tips to elevate your documentation skills.
Why Nurse Notes Matter
Nurse notes serve as a communication tool between healthcare providers, ensuring everyone is on the same page regarding patient care. They also act as legal records, protecting nurses and healthcare facilities in case of disputes. Accurate documentation is non-negotiable, as it directly impacts patient safety and treatment efficacy.
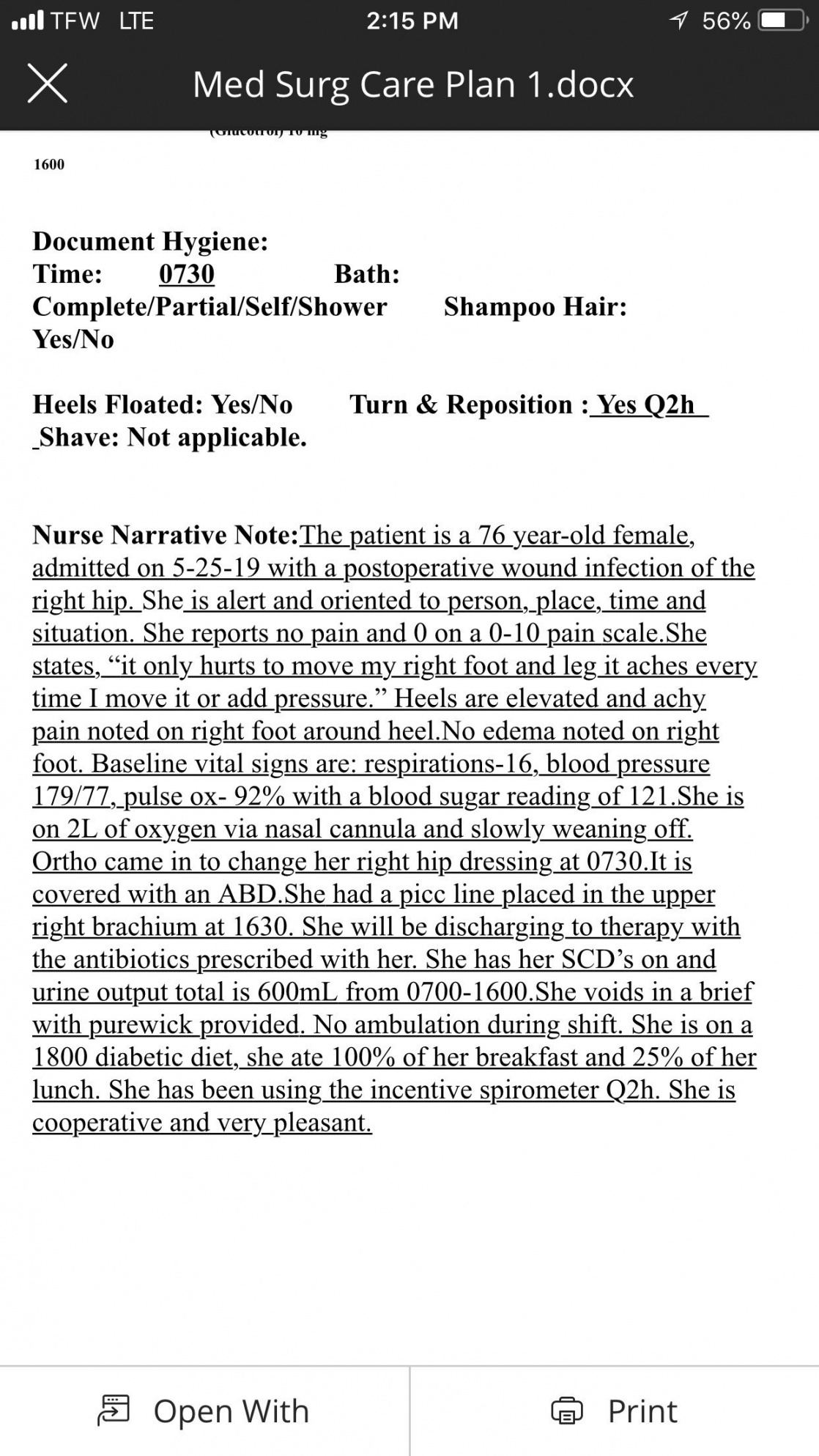
Real-Life Example of Nurse Notes

Here’s an example of well-structured nurse notes:
Patient: John Doe
Date/Time: 05/15/2023, 08:00 AM
Assessment: Patient reports mild pain (3⁄10) in the left leg. Vital signs: BP 120⁄80, HR 72, RR 18, Temp 98.6°F. Wound dressing intact, no signs of infection.
Intervention: Administered 500mg of acetaminophen PO for pain relief. Encouraged ambulation as tolerated.
Outcome: Patient ambulated 50 feet with a walker, reporting pain reduced to 2⁄10.
📝 Note: Always use objective language and avoid subjective terms like "seems" or "appears" unless necessary.
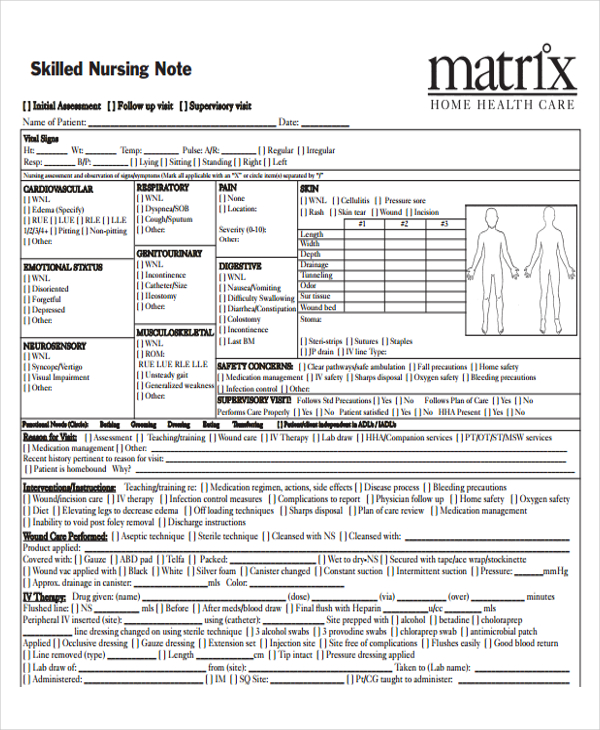
Key Components of Nurse Notes
Effective nurse notes include:
- Patient Identification: Name, room number, and date/time.
- Assessment: Objective findings and patient-reported symptoms.
- Interventions: Actions taken, medications administered, or treatments provided.
- Outcomes: Patient response to interventions.
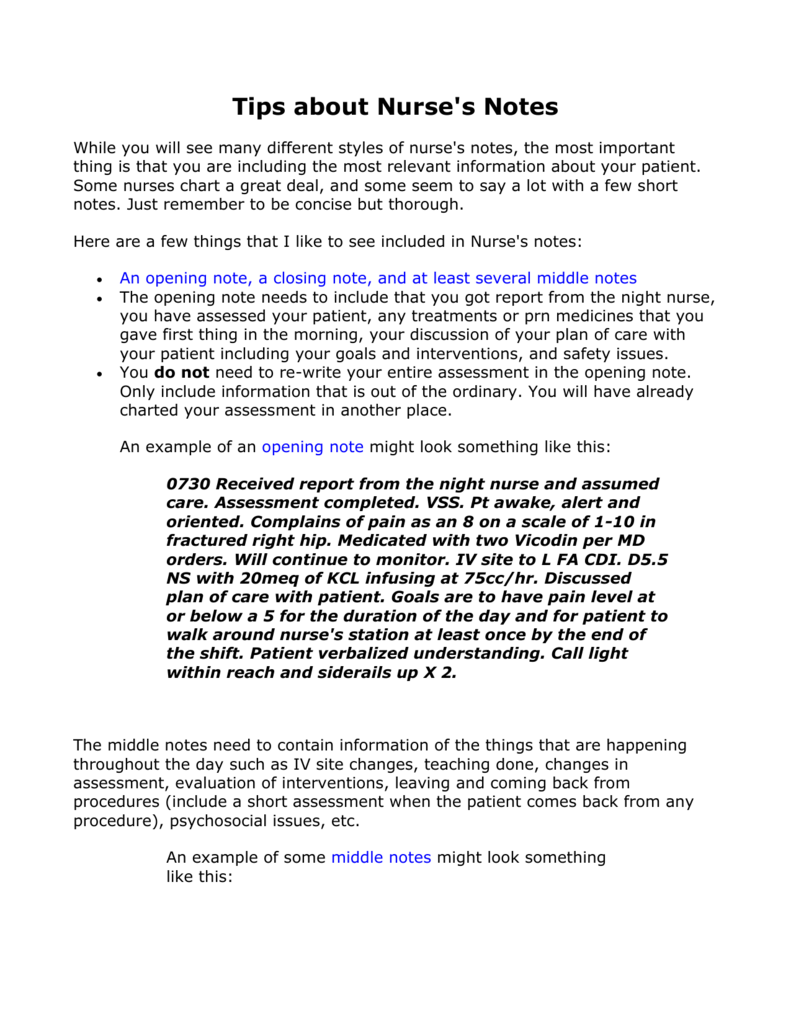
Tips for Writing Clear Nurse Notes

- Be Concise: Stick to relevant details.
- Use Standard Abbreviations: Avoid jargon or unclear shorthand.
- Document Timely: Record observations and actions promptly.
- Focus on Facts: Avoid assumptions or opinions.
| Do’s | Don’ts |
|---|---|
| Use objective language | Include personal opinions |
| Document all interventions | Omit critical details |
| Follow facility guidelines | Use non-standard abbreviations |
Common Mistakes to Avoid

- Incomplete Documentation: Missing key details like time or dosage.
- Late Entries: Delaying documentation can lead to inaccuracies.
- Inconsistent Formatting: Stick to your facility’s standards.
⚠️ Note: Inconsistent documentation can lead to legal issues and compromised patient care.
Checklist for Perfect Nurse Notes
- [ ] Include patient identification details.
- [ ] Record objective assessments.
- [ ] Document all interventions and medications.
- [ ] Note patient responses and outcomes.
- [ ] Review for accuracy and clarity.
Enhance Your Documentation Skills
Investing in nurse documentation tools or templates can streamline your workflow. Many healthcare facilities offer training programs to improve documentation practices.
What should I include in nurse notes?
+Include patient identification, assessment, interventions, and outcomes. Be concise and objective.
How often should I update nurse notes?
+Update notes after every significant interaction or change in the patient’s condition.
Can I use abbreviations in nurse notes?
+Yes, but only use standard, approved abbreviations to avoid confusion.
Mastering nurse notes is crucial for delivering high-quality care. By following best practices and learning from real-life examples, you can ensure your documentation is accurate, clear, and compliant. Remember, effective nurse notes not only protect you legally but also improve patient outcomes.
nurse documentation,nursing notes examples,nursing documentation tips,patient care documentation,nursing best practices